Osteoarthritis of the hip (Part two)
Treatment
What can be done for this condition?
Non-surgical treatment
Osteoarthritis, unfortunately, is a condition that cannot be cured. There are various therapies that make it possible to relieve symptoms, slow down further degeneration of the cartilage, and improve the quality of life of patients.
Your doctor may prescribe some medications to help control pain. Acetaminophen, a medication with few side effects, helps in relieving pain. Some people may find pain relief with anti-inflammatory drugs, such as ibuprofen and aspirin. Newer anti-inflammatory medications of the "COX-2 inhibitor" class have shown promising results and do not cause stomach upset or other intestinal problems.
Medical studies have shown that glucosamine and chondroitin sulfate may also help in osteoarthritis of the hip. These supplements seem to help similarly to anti-inflammatories, with fewer side effects. Many doctors think that research supports these supplements and encourage their patients to use them.
If pain is not relieved with the use of the above-mentioned medication classes, the use of stronger medication classes such as cortisone is possible. Cortisone is a powerful anti-inflammatory medication, but it has side effects that limit its use in treating osteoarthritis. Multiple cortisone injections relieve pain but accelerate the degeneration process.
Repeated injections also increase the risk of developing infections in the hip joint. Every time a needle is inserted into a joint, there is a possibility of infection. Most doctors use cortisone with great caution. They try to avoid multiple injections. If the joint is in the final stages of degeneration and artificial hip replacement is inevitable, cortisone may be used to relieve pain.
Physical therapy plays a critical role in the non-operative treatment of hip osteoarthritis. The primary goal is to help you learn to control symptoms and maximize your hip's health.
Surgical intervention
In some cases, surgical treatment of osteoarthritis may be necessary.
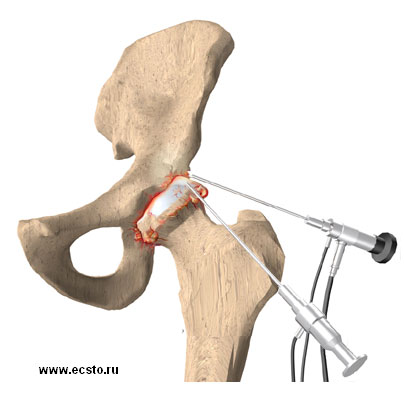
Arthroscopy
Surgeons may use an arthroscope to check the condition of the articular cartilage. The arthroscope is a small TV camera that is inserted into the joint through a small incision. By checking the condition of the cartilage, the surgeon may try different techniques to soothe the pain. One method involves cleaning the joint by removing loose cartilage fragments. Another method involves applying a saline solution to the joint, after which patients report pain relief.
This procedure is sometimes useful for temporary relief of symptoms. Hip arthroscopy is a relatively new method, and it is still unclear which patients benefit from this method.
Osteotomy
When the placement of the hip changes due to disease or trauma, more pressure than normal is exerted on the joint surfaces. This extra pressure leads to more pain and faster degeneration of the joint surfaces.
In some cases, surgery to rebuild the angles of the pelvic socket or femur (thigh bone) may result in shifting the pressure to other healthy parts of the hip joint. The goal is to spread the forces over a larger surface in the hip. This may help to ease pain and slow down further degeneration.
Procedures to rebuild the angles of the joints are called osteotomies. In this procedure, the bone of the pelvic socket or femur is cut, and the angle of the joint is changed. The procedure is not always successful. Generally, it will reduce your pain but not completely eliminate it. The advantage of this procedure is that very active people can still have their own hip joint and once the bones heal, there are fewer restrictions regarding activities.
An osteotomy procedure under the best circumstances is most likely only temporary. It is thought that this operation extends the time before a total hip replacement is necessary.
Artificial hip replacement
Arthroplasty or artificial hip replacement is the ultimate solution for advanced osteoarthritis. Arthroplasty is one of the most effective surgeries that modern medicine has evolved. If a few years ago arthroplasty was performed in patients older than 60 years, modern medicine has evolved the types of metals, the types of friction forces, and the strength of the artificial joint making arthroplasty a very effective method even for younger patients.
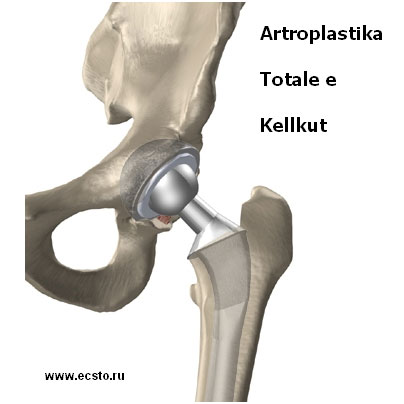
Arthroplasty is divided into several types. It can be total, which means replacing all the components of the hip joint. In such cases, both the acetabular and femoral elements are replaced. Depending on the type of osteoarthritis, the patient's age, their profession, body anatomy, and many other factors, the choice of the type of artificial joint used is made.
Partial (or subtotal) arthroplasty means partial replacement of the hip joint. That is, only the femoral element is replaced while leaving the acetabular element untouched. There are also other arthroplasty modifications like "resurfacing", which itself means replacing the joint while leaving part of the femur's neck untouched.
After surgical intervention
Immediately after the surgery, I will visit you in your room at the hospital. You will practice getting out of bed and walking using a walker or a pair of crutches. Exercises are used to improve muscle tone and strength in the thigh and hip muscles and to help prevent the formation of blood clots.
During healing, you must follow the surgeon's instructions on how much weight you can put on the operated limb while standing or walking. Once you return home from the hospital, the surgeon may suggest working with a physical therapist for up to six weeks at home.
These visits are conducted to ensure that you are safe inside and outside the house, inside or outside the car. The therapist makes suggestions regarding your safety, reviews special measures for the hip, and ensures that you have placed a safe amount of weight on your leg during standing or walking. Home therapy ends when you can safely leave the house.
Some additional visits to outpatient physical therapy may be necessary for patients who still have problems walking or who need to return to heavy physical work or activities.
The goal of the therapist is to help you control the pain, regain the normal walking pattern, and perform activities without risking further damage to the hip. When you are on the path to recovery, regular visits to the therapist's office will end. The therapist will continue to be an important resource, but you will need to carry out exercises as part of an ongoing program at home.