Osteoarthritis and Hip Arthroplasty (Part Two)
In order for us to have a clearer understanding of what was mentioned above, let's take a clinical example. Patient X, 38 years old – athlete. Complaints at the time of consultation with me: pain in the inguinal area and the back part of both limbs during walking.
Over the last 6 months, a minimal shortening of the right limb is noticed. Limping while walking. Was treated for a long time with conservative therapy and physiotherapy, which was ineffective. I recommend for the patient arthroplasty of the hip joint, replacing it with an artificial joint.
My duty and that of every surgeon is the step-by-step planning of the operation stages. The first necessary and essential thing is the pelvis radiography (fig 1) and the radiography of the damaged hip. The diagnosis that I set in this case is: Avascular necrosis of both femur heads.
From the radiographs, a clear bilateral deformity of the femur heads is visible. The bone density is reduced (has become soft), narrowing of the joint path and damage to the joint cartilage is clearly visible. What prosthesis will we use in this case?
There are 3 key moments that we need to keep in mind. The first is the patient's young age. The second is the fact that the patient is an athlete. And the third is the radiography of the hip. From investigations and observations over many years of implanted prostheses, the friction forces that have shown the greatest strength are metal-metal. So if the head of the prosthesis will be metallic and the accessory of the acetabular element will be metal, we will have a rigid friction force. Rigid forces at the same time have their own disadvantages.
Scientific data have shown that metal ions that detach as a result of friction in the joint lead to a condition called metallosis. So, the entire area around the joint is filled with metal ions. There have been cases where patients after many years are diagnosed with various pseudotumors. In recent years, metal-metal friction force prostheses are preferred to be coated with a kind of layer called oxinium. This layer is believed to bring good results and the cases of metallosis and pseudotumors will be much lower.
The first thing we will keep in mind is that for an athlete who claims to continue in his life to engage in sports, we will implant a metallic head with a metallic acetabular accessory with an oxinium layer. Another friction force that is very preferred and used extensively are ceramic-ceramic forces. The truth is that they are not as strong as metal but have shown very good results.
If the patient does not think that in his life he will engage in sports and will not lead a "super-active" life then we will recommend for him a ceramic head prosthesis with a ceramic socket. Ceramics have shown very good results. If compared with metal, no tumor cases or similar complications have been observed. So, the choice of friction force for me is one of the key points in the choice of the prosthesis.
The second moment is the choice of the fixation of the prosthesis stem. For a young patient, I would not recommend prostheses with cement fixation. If we look at the statistics, a dominant percentage of orthopedists prefer prostheses with "press-fit" fixation.
The fixation of the prosthesis stem and the acetabular element with cement complicates things in the future for a young patient. It should be taken into account that in case a reimplantation of the prosthesis is needed, during the extraction of the prosthesis a large part of the bone mass is damaged. In other words, a large defect is created both in the femoral bone and in the acetabulum. For our case, we will choose a prosthesis with "press-fit" fixation.
As we mentioned above, to achieve a surgical intervention we do pre-operative planning. For our 38-year-old patient with a diagnosis of bilateral avascular necrosis, an athlete who claims to continue to engage in physical exercises in the future, we chose a prosthesis with metal-metal friction forces, the head of which will be coated with an oxinium layer. We will choose the leg of the prosthesis with proximal fixation without cement. It will be wide and short, which will give us the opportunity to implant it without damaging the femoral canal much.
Once we have a detailed pre-operative plan, once we have chosen the type of prosthesis to be used along with the preliminary sizes of each component, we can say that we are ready to perform the intervention.
Some of the incisions used for the hip transplant are: posterior incision, lateral, antero-lateral, anterior and some other modified versions. In my practice, I prefer to use the modified lateral incision. The incision is made at the level of 1 cm above the major trochanter continuing 40-45 degrees on the anterior side. At this level, once we have reached the major trochanter, the gluteus medius muscle will be clearly visible. The key point of this modified incision is the partial detachment of the gluteus medius muscle from the major trochanter, which will clearly open the horizon of the neck of the hip joint.


The length of the incision is necessary as much as we have the opportunity to extract the femur head from the acetabular cavity. In our case, an incision of 70-80mm will be sufficient to perform the transplant of the joint. This kind of incision can truly be called minimally invasive.
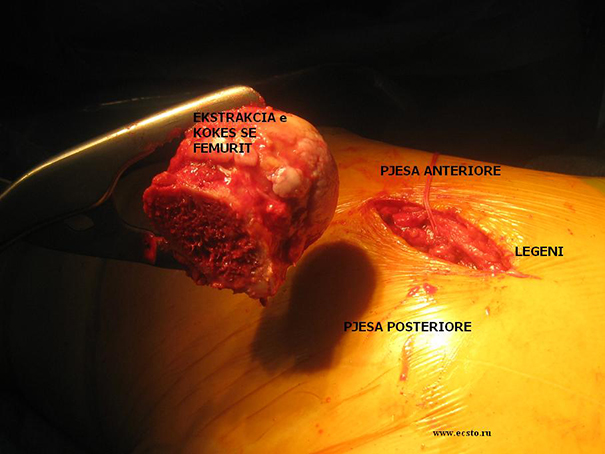
This is a view from the femur head of the damaged hip. The damaged cartilage part and avascular necrosis of the femoral head are very clearly visible.

After making the cuts and extracting the head, we will have an open horizon to work with the acetabulum of the hip where the acetabular element will be implanted.
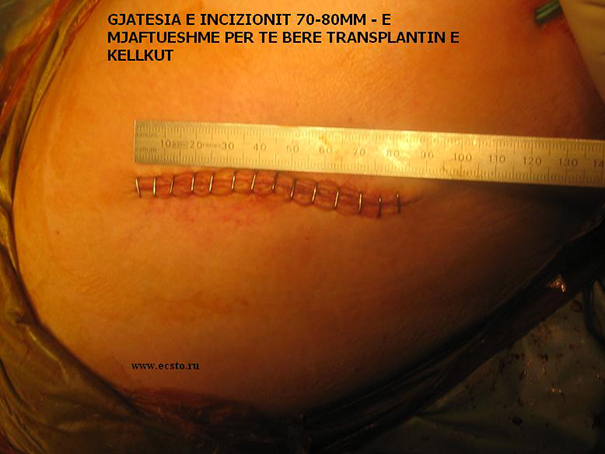
After implanting the artificial joint, we can call the arthroplasty successful. We measured the length of the incision – it is about 80mm.

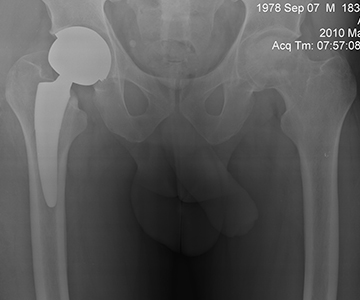
After the operation, it is necessary to have a radiography of the pelvis where both hip joints are clearly visible and the radiography of the hip that we just operated on. Generally, in my practice, the patient stands up and walks on his own the second day after the operation.
Hello! I also have such a problem and wanted to know how much the operation might cost
Sent by Rezarta Cakerri, më 14 January 2014 në 01:44
Hello! How much does such a surgery cost? The patient is a 74-year-old woman
Sent by Thanas Gjyli, më 01 May 2014 në 03:19