Pre-Implantation Genetic Diagnosis (PGD)
Pre-implantation genetic testing as part of Assisted Reproduction Techniques (ART) is a technique used to identify genetic defects in embryos created before pregnancy occurs. This is done with the help of Artificial Fertilization or otherwise known as IVF. The testing is performed on the embryo (the union of the egg with the sperm) to determine if the embryo carries genetic abnormalities. After the result from the genetic laboratory, only the embryos that are found normal (without genetic abnormalities) are transferred to the female’s uterus hoping for a pregnancy.
The technique is used mostly in two patient groups: The first group are individuals at high risk of having a child with a genetic disease, e.g., carriers of a single gene disease or structural chromosomal aberrations, such as translocations. These patients have continuously interrupted pregnancy based on prenatal analyses, have infertility at the same time (congenital bilateral absence of the vas deferens), or have frequent miscarriages (which is common in carriers of translocations).
The second group are those who have been treated with artificial fertilization (IVF), who may have a low risk of genetic abnormalities but their embryos are analyzed for chromosomal aneuploidy (a disorder in the number of chromosomes) to increase the chance both for achieving and continuing the pregnancy. This is mostly applied when the patient has several failed IVFs and the cause is thought to be a chromosome number anomaly in the formed embryos or when the patient is of such an age like over 37 years old when these anomalies are thought to increase.
Pre-implantation genetic testing is an alternative to diagnostic procedures that are performed after conception (e.g., amniocentesis or chorionic villus sampling), which are often followed by the difficult decision of terminating the pregnancy if the result is not favorable.
PGD is currently the only option to avoid the high risk of having a child affected by a genetic disease before the embryo is implanted and pregnancy is formed. However, performing this technique does not mean that prenatal tests should not be performed since it has been noticed that abnormalities can occur in the fetus even from external factors such as tobacco, used medications, etc., even after pregnancy is established.
The PGD technique was first reported in the United Kingdom in 1990, sparking a major debate about its use. Over the years, with the perfection of the technique and the respective legislation, this technique is routinely performed in all countries, helping many couples who did not have this possibility before.
In the same line have also advanced the techniques used to analyze chromosomal abnormalities. Initially, the PCR (polymerase chain reaction) technique was used, which tests a single chromosome. Later, it was seen necessary to use the FISH (fluorescent in situ hybridization) technique, which analyzes several chromosomes at the same time. Most recently, it has been possible through the CGH (Comparative Genomic Hybridization) technique to analyze all chromosomes in certain patients where it is deemed necessary.
How is PGD performed?
The PGD procedure is performed as follows:
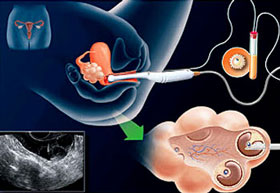
Step 1. In vitro fertilization is performed – if every menstrual cycle the female usually produces one mature egg during the procedure she is stimulated to produce at least 3 mature eggs. Once a certain moment arrives, through a mini-invasive intervention, the eggs are taken by the gynecologist (fig. 1) and pass under the supervision of the embryologist who after finding and "stripping" them from cells that are no longer needed assesses their maturity. At the same time, the husband provides the sperm material which is processed in a way that selects the best spermatozoa. On the same day, the union is carried out using the ICSI (intra-cytoplasmic sperm injection) technique which has the principle of one egg-one spermatozoon (fig.2).
 |
 |
| Fig 1. The process of taking the eggs | Fig 2. The process of performing ICSI |
Step 2. The embryos are grown in the laboratory in conditions that mimic the natural conditions of the uterus until the third day when it is in the 8-cell stage.

Fig 3. Embryo in the third day stage and the process of removing a cell (blastomere)
Step 3. At this stage, the embryologist performs the procedure by removing one or two cells (blastomeres) from the embryo (fig.3). It should be emphasized that genetic analysis can be performed at any stage of embryo development. We apply the technique at the third day stage as the results have been seen much better at this stage.
Step 4. The cells under very special conditions are sent to the genetic laboratory where they are subjected to genetic analysis to see if the embryo from which they were removed carries genes that cause the family’s genetic disease.
Step 5. On the fourth day of development, the answer comes from the genetic laboratory.
Step 6. On the fifth day of development, only the healthy embryos are transferred into the uterus to allow them to develop (fig.5).
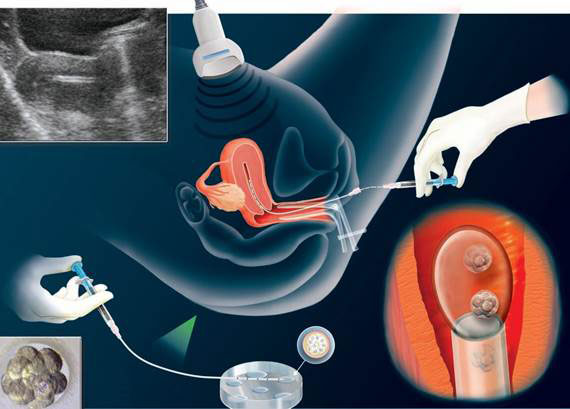
Fig 5. The process of performing embryo transfer.
Step 7. About 12 days after the embryo transfer, the woman takes a β-HCG blood test to see if she is pregnant.

The PGD technique as well as all other Assisted Reproduction Techniques (ART) have been performed for years by a specialized team of embryologists at the American Hospital in Tirana and recently with the opening of the In-Vitro Fertilization department in Pristina, achieving successes that have helped many couples who were directed abroad to undergo this procedure.