Ear Diseases (Part Three)
Clinical Signs.
- Otorrhea in small quantities and with a very bad smell is always purulent and never mucoid.
- A progressive decrease in hearing is observed.
- Ear pain and fever in cases of acute reinfections.
- Headache and a feeling of pressure in the head.
Diagnosis. Cholesteatoma is divided into secondary cholesteatoma of the middle ear called tensa cholesteatoma develops from retraction pockets as a result of chronic infections at the level of the marginal perforation in the posterior-superior quadrant of pars tensa and primary cholesteatoma called flaccid cholesteatoma arises from the growth of keratinized squamous epithelium at the level of pars flaccida under the presence of chronic inflammatory stimulation in the epitympanum which promotes the proliferation of squamous epithelium. The small perforation often created is usually covered by a crust while continuing to destroy the lateral wall of the attic, which is characteristic of this type of infection.
The appearance of medial granulations, the bad smell of secretions, and the white color of the cholesteatoma are signs of the disease during the otoscopic examination of the ear. The patient presents conductive hearing loss and in advanced stages, the inner ear is also involved. Occult cholesteatomas are those cases when cholesteatoma develops in the middle ear behind a normal tympanic membrane.
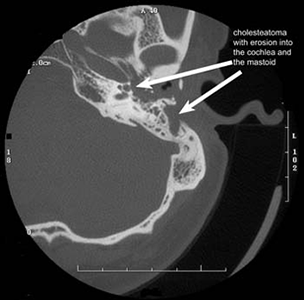
A great diagnostic help is provided by axial and coronal CT which gives good information about bone destruction, soft tissue abnormalities in the tympanic cavity, and the extension of the cholesteatoma into the cranial cavity.
Treatment. Conservative treatment through the use of antibiotics and corticosteroids in ear drops is ineffective. Surgical treatment consists of radical removal of the inflammation and reconstruction of the middle ear.

Extra and Endocranial Complications originating from the ear.
Complications originating from the ear must be diagnosed as quickly as possible and their treatment must be immediate. Clinical, audiometric, neurovestibular examination, radiological CT examination should be performed as quickly as possible. Surgical treatment has a higher priority.
Labyrinthitis.
Clinical Signs. Dizziness, nausea, vomiting, ringing noises in the ear, deafness that sets in for a short period. The patient has no fever and no pain.
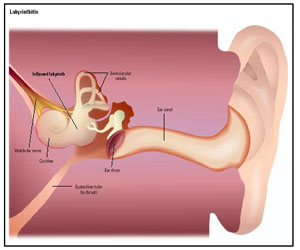
Pathogenesis.In some forms of acute otitis, toxins spread to the labyrinth through the windows located in while the infection passes into the labyrinth through the blood vessels. In cases of chronic middle ear otitis with cholesteatoma, the infection spreads into the labyrinth through fistulas created in the perilymphatic space. The infection can also be superimposed after a surgical trauma or after a trauma accompanied by transverse fractures of the temporal bone.
Diagnosis. The patient has all the signs of severe damage to the inner ear.
Differential Diagnosis. Meniere's disease, sudden deafness, acute vestibulopathy.
Treatment. Immediately starts with high-dose intravenous antibiotics continuously accompanied by radical mastoidectomy in cases of chronic middle ear otitis with cholesteatoma. In cases of trauma, surgical intervention is undertaken in cases of massive cerebrospinal fluid otorrhea, facial nerve paralysis, and meningitis.
Prognosis. Labyrinthitis appears in clinical forms with different courses depending on the development of the pathological process. Serosal labyrinthitis usually appears after traumas or viral conditions, purulent forms are caused as a result of the invasion of the perilymphatic space by bacteria, circumscribed forms in cases of labyrinth fistulas as a result of cholesteatoma, and generalized when the entire labyrinth is involved in the process as a result of the continuation of the infection spread in it or this situation may also come as a result of a generalized infection. In the late forms, the disease follows a fulminant course with complete irreversible loss of the inner ear functions. The infection is capable of extending towards the meninges.
Epidural Empyema.

Clinical Appearance. Monotonous pulsating headache, otorrhea, subfebrile temperature. There are no typical characteristic pathognomonic signs for the disease.
Pathogenesis. Acute or chronic infections spread from the mastoid process towards the subdural space as a result of the destruction of the bone wall that separates the middle ear from the endocranial cavity.
The infection can also spread through the blood vessels that cross the bone wall which may remain intact.
Diagnosis. There are few characteristic symptoms for this disease, sometimes it can be discovered during mastoidectomy surgery. Diagnosis can be a result of radiological examinations such as CT, MRI.
Treatment. Immediate mastoidectomy with exposure of the dura within healthy limits, drainage, and antibiotic therapy.
Prognosis. It is good when the disease is caught and treated quickly; otherwise, there is a risk of developing paucimeningitis advancing to leptomeningitis. Subdural empyemas are rare and come as a consequence of diffuse meningitis.
Otogenic Meningitis
Clinical Signs. Include severe headaches, stiff neck implying inability to bend the neck and body, consciousness progressively darkens, photophobia, irritability, tonic-clonic seizures, facial paralysis. Otorrhea, otalgia, and deafness may be absent or occult. Typical are rapid pulse, irregular breathing, high temperature. The patient may present paralysis of the oculomotor or abducens nerve and display abnormalities in the eye fundus.
Pathogenesis. The cause is the spread of an acute or chronic infection, usually caused by pneumococcus, towards the subarachnoid space.
- Directly as a result of bone destruction from infection.
- Through the blood vessels or nerves that penetrate the bone wall.
- Through the continuation of the spread of thrombophlebitis of the veins.
- Through the labyrinth in these cases serves the internal acoustic meatus.
Diagnosis. In these cases, we have the typical signs of acute meningitis where typical indicators in cases of cerebrospinal fluid meningitis are found, signs of an acute, subacute, and in most cases chronic ear infection of various degrees of external manifestation. Radiological examinations may be decisive for diagnosis and in choosing the treatment method.
Differential Diagnosis. Includes viral meningitis or epidemic meningococcemia as well as tubercular meningitis.
Treatment. Use of high-dose antibiotics based on antibiogram. The use of penicillin from 20-60 million IU per day is recommended in cases of infection by pneumococcus. Repeating lumbar puncture should be done to evaluate the effectiveness of the treatment.
Prognosis. The disease may end fatally in untreated or poorly treated cases. The prospect of recovery exists in 90% of cases when diagnosed early as the cause is otitis media and appropriate treatment is started immediately.