Ear Diseases (Part Five)
Clinical Signs Depending on the location of the otosclerosis focus, we have the clinical presentation.
- Conductive hearing loss in 85% of cases when the focus is in the middle ear.
- Mixed hearing loss in 15% of cases which implies both conductive and sensorineural hearing loss.
- Pure sensorineural hearing loss in 5% of cases.
The disease develops gradually, accompanied by progressive hearing loss which initially affects one ear and over time also affects the other ear in most cases. The patient begins to constantly feel a progressive noise in the ear.
The disease never causes otalgia, otorrhea, dizziness, or balance disorders.
Pathogenesis. Otosclerosis involves a localized disorder of bone minerals or metabolism, which is accompanied by an increase in enzymatic activity of mesenchymal cells in the labyrinthine capsule, mainly genetic factors predominate but also hormonal disorders contribute.
- Family history.
- Through otoscopy, we can observe a hyperemic zone in the promontory called the (Schwartze) sign
- Functional tests, in the tonal audiogram, show a conductive hearing loss, sometimes mixed loss, and rarely sensorineural loss. Characteristic is the Carhart notch, which indicates a bone hearing loss at the frequency of 2000Hz. In tympanometric examination, we notice a curve with normal shape but slightly low amplitude and the absence of the stapedius reflex as a result of the fixation of the stapes base.
- Radiological examination shows very good pneumatization of the mastoid.
Differential Diagnosis
- Made with congenital anomalies of the middle ear.
- With the disarticulation of the ossicular chain after traumas.
- Post-inflammatory fixation of the hearing bones.
- With adhesive processes.
- Tympanosclerosis.
Treatment. The only treatment remains surgical. And there are two types of operations: stapedectomy, which implies the removal and exposure of the stapes and the fixed base which is removed and replaced with a prosthesis prepared with fat, cartilage etc., that is fixed to the lenticular process of the incus. We also have Stapedotomy, which implies the opening of a hole at the base of the stapes and the placement of an industrial prosthesis that depends on the long or lenticular process of the incus and the piston is fixed to the hole we have punctured.
Prognosis. The disease is manifested in 70% of cases by the ears. Both ears can be operated on with a time interval of about 6 months. In cases where the patient presents with severe sensorineural hypoacusis, surgery in the better hearing ear is not indicated.
Vestibular disorders or dizziness.
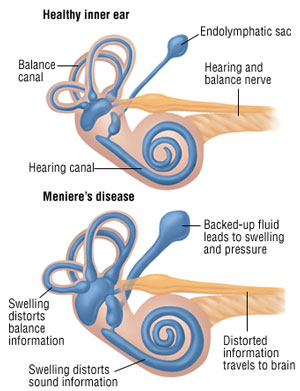
Meniere's Disease
Clinical Signs. The classic triad was described for the first time by Meniere in 1861 and includes.
- Continuous noise in the ear with low frequency that changes intensity.
- Immediate hearing loss.
- Dizziness in the form of attacks with a feeling of spinning objects.
A typical attack begins acutely with the triad described above followed by nausea, vomiting, and other vegetative symptoms. The patient feels a blockage in the ear. Noise in the ear and hearing loss may begin before the attack and change during it.
Characteristic is that tinnitus or ear noise improves while hearing deteriorates and in most cases improves after the attack, and this is called the “Lermoyez phenomenon”. Symptoms are usually unilateral, in most cases after the attack hearing normalizes and the noise disappears from the ear.
In the later stages of the disease's development, a permanent hearing loss for low tones is observed, and in the final stage, the hearing loss is unilateral, severe, and for all frequencies. The cause of the disease's manifestation is not clear.
Pathogenesis. The disease appears as a result of the disruption of the quantitative balance between perilymph and endolymph volumes, resulting in qualitative changes in the electrolyte content between perilymph and endolymph through the process of osmotic pressure throughout the entire membranous labyrinth. This causes endolymphatic hydrops.
Treatment.
During the attack.
- Lying down in bed.
- Intravenous solutions with electrolytes in cases of severe vomiting.
- Intravenous antiemetic and antivertigo medications.
- Solutions with small molecular weight such as dextran and vasodilators to improve the circulation of the labyrinth and to enhance the circulation of perilymph and endolymph